Sexual dysfunction (SD) is a frequently underestimated complication of multiple sclerosis (MS), yet it affects nearly two-thirds of patients across their disease trajectory. Its impact is not confined to the bedroom; it extends into domains of mood, self-esteem, relationships, and overall quality of life. Importantly, SD is not a uniform entity. It encompasses primary neurological disturbances, secondary effects from MS-related disabilities, and tertiary psychosocial burdens. Effective management thus requires a multifaceted and personalized approach.
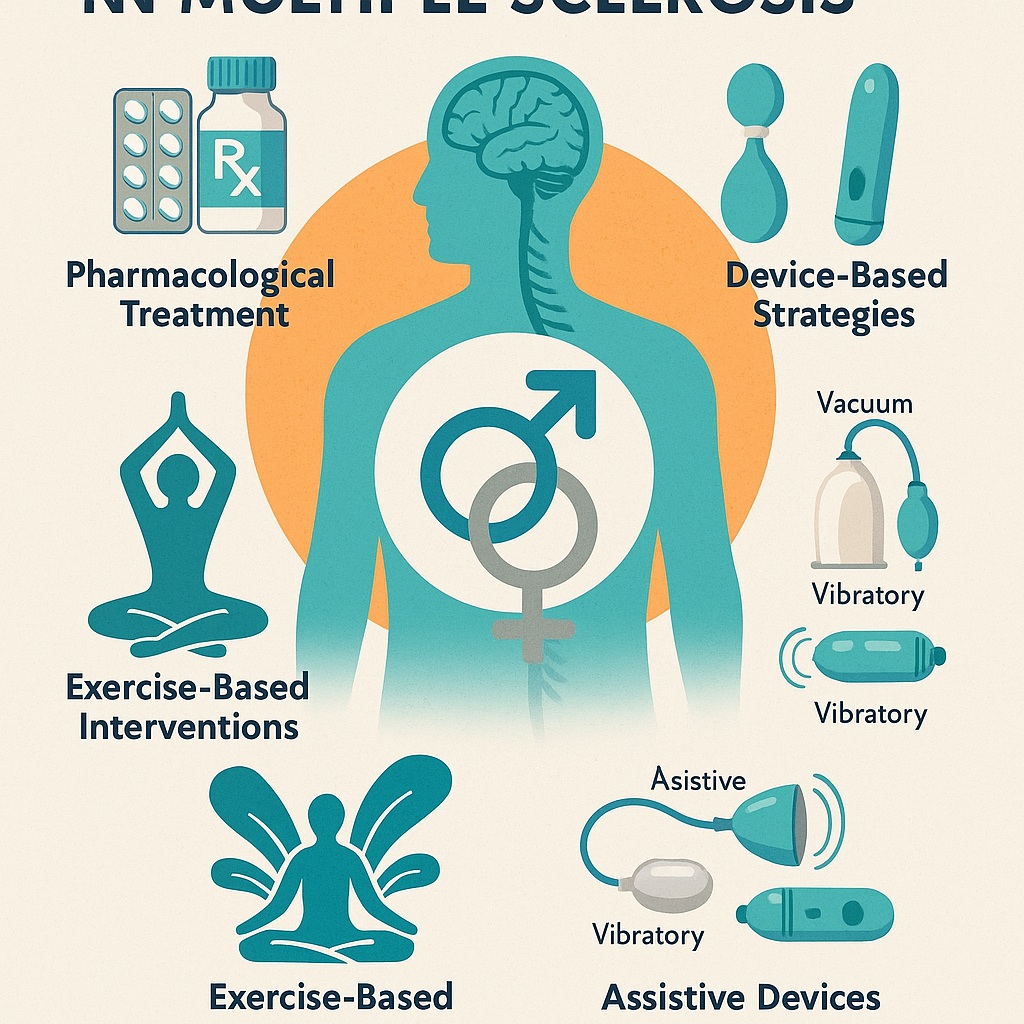
This article synthesizes evidence from recent clinical research—including systematic reviews of both pharmacological and non-pharmacological interventions—and explores practical strategies for clinicians. Special attention is given to the evolving role of sildenafil and related agents, alongside integrative therapies such as pelvic floor training, aquatic exercise, yoga, and assistive devices.
The Hidden Burden of Sexual Dysfunction in MS
Sexual health is rarely the first priority in neurological consultations, yet in MS it deserves more attention than it often receives. Approximately 50–90% of men and 40–80% of women with MS report SD, manifesting as erectile dysfunction, diminished libido, orgasmic difficulty, impaired vaginal lubrication, or spasticity interfering with intimacy. Unlike many neurological symptoms, SD carries a heavy psychological toll, often outweighing the physical burden of MS itself.
Patients commonly report that sexual dysfunction contributes more to their sense of disability than fatigue or gait impairment. This finding is sobering: a disease that robs mobility also disrupts one of the most intimate aspects of human connection. The stigma surrounding sexual issues further silences patients, while physicians often hesitate to inquire. As a result, SD in MS remains underdiagnosed and undertreated despite its clear impact on mental health and life satisfaction.
Recognizing SD as a legitimate medical symptom, rather than a peripheral complaint, is the first step toward effective intervention.
Pharmacological Interventions: Promise and Limitations
Sildenafil and PDE5 Inhibitors
The most studied pharmacological option remains sildenafil, the archetypal PDE5 inhibitor. By enhancing nitric oxide–cGMP signaling, sildenafil restores cavernosal smooth muscle relaxation and penile blood flow. While sildenafil revolutionized the treatment of erectile dysfunction in the general population, its efficacy in MS-related ED is mixed.
A landmark study showed that sildenafil produced little benefit compared with placebo in men with MS, leading to the conclusion that it should not be considered routine therapy for MS-related ED. The likely explanation lies in the neurological basis of dysfunction: when nerve conduction pathways are compromised by demyelination, vascular enhancement alone may not suffice.
Other PDE5 inhibitors, such as tadalafil, show somewhat more promise. In one trial, daily 5-mg tadalafil improved erectile scores and even reduced lower urinary tract symptoms in men with active MS. This dual benefit highlights the therapeutic potential of PDE5 inhibition but also underscores the variability in response between individuals.
OnabotulinumtoxinA
For women with MS, intradetrusor injections of onabotulinumtoxinA demonstrated improvements not only in bladder control but also in sexual satisfaction, including desire, arousal, lubrication, orgasm, and overall quality of life. The mechanism is thought to involve a combination of urological relief and psychological confidence, underscoring the interconnected nature of sexual health.
These findings suggest that pharmacological therapy has a place in MS-related SD but cannot be the sole solution.
Exercise-Based Interventions: Reclaiming Function Through Movement
Aquatic Exercise
Water-based therapy offers a safe, low-impact environment for patients with MS, who often struggle with mobility limitations, heat sensitivity, and fatigue. Clinical studies show that aquatic exercise performed two to three times per week for eight weeks significantly improved sexual function scores, particularly in domains of desire, arousal, and orgasm. Interestingly, twice-weekly sessions appeared more beneficial than thrice-weekly, perhaps due to reduced fatigue.
Beyond physical outcomes, aquatic therapy improved mood, reduced depressive symptoms, and enhanced partner satisfaction. It represents a holistic intervention that simultaneously addresses neurological, psychological, and relational dimensions.
Pelvic Floor Exercises
Pelvic floor muscle training (PFMT) is another cornerstone of non-pharmacological therapy. For women with MS, structured PFMT programs led to improvements in desire and orgasm. When combined with electromyograph biofeedback or neuromuscular stimulation, benefits were even greater.
In men, however, evidence is less robust, with some studies showing minimal benefit. Nevertheless, PFMT remains a valuable adjunct, especially for addressing urinary incontinence—a symptom intricately tied to sexual health and self-esteem.
Mind-Body Approaches: Yoga and Mindfulness
Yoga
Yoga interventions, particularly those lasting 12 weeks or longer, showed improvements in sexual satisfaction and overall quality of life in women with MS. The benefits extend beyond the physical, incorporating elements of mindfulness, body awareness, and stress reduction. Given the fatigue and anxiety burden in MS, yoga serves as both therapy and coping strategy.
Mindfulness
The integration of mindfulness with pelvic floor exercise produced mixed results. Some studies reported no significant difference compared to either intervention alone, highlighting the need for larger, more controlled trials. Still, mindfulness remains attractive as a safe, low-cost adjunct that may empower patients to reclaim agency over their sexual well-being.
Assistive Devices: From Vacuum to Vibration
In select cases, technology can bridge neurological deficits. The clitoral vacuum suction device (CVSD) demonstrated improvements in orgasm and overall sexual function among women with MS, outperforming vibratory devices in some domains. Vibratory stimulation, while effective for orgasm, produced less sustained benefit for overall sexual satisfaction.
For men, vacuum erection devices remain a viable mechanical aid when pharmacotherapy is insufficient. Importantly, these devices should not be relegated to “last resort” status but presented as legitimate, evidence-based options.
Integrating Therapies: Toward a Holistic Framework
What becomes clear from reviewing pharmacological and non-pharmacological strategies is that no single approach universally resolves MS-related sexual dysfunction. Instead, the most promising outcomes emerge when therapies are integrated: sildenafil for vascular support, pelvic floor training for muscular reconditioning, aquatic therapy for holistic health, and psychological support for mood and relationship resilience.
This integrated framework requires collaboration across specialties. Neurologists, urologists, gynecologists, physiotherapists, psychologists, and sexual health counselors must work in concert. Only then can therapy address the primary neurological deficits, the secondary consequences such as fatigue and incontinence, and the tertiary psychosocial barriers to intimacy.
Challenges and Research Gaps
Despite encouraging results, several limitations persist:
- Small sample sizes: Most studies enrolled fewer than 100 patients, limiting generalizability.
- Heterogeneity: Differences in MS subtype, disease duration, and disability levels complicate interpretation.
- Short follow-up: Few trials extended beyond 12 weeks, leaving long-term efficacy unknown.
- Self-reported measures: Reliance on subjective questionnaires introduces bias and underreporting due to stigma.
Future research should prioritize larger, multicenter randomized trials with standardized outcome measures and longer follow-up. Incorporating objective physiological assessments, such as penile elastography or transvaginal ultrasonography, may provide more reliable endpoints.
Conclusion: Restoring Sexual Health in MS
Sexual dysfunction in MS is neither inevitable nor untreatable. While no universal cure exists, the growing body of evidence supports a multimodal approach: start with lifestyle and exercise-based interventions, integrate assistive devices when needed, and use pharmacological therapies such as sildenafil or onabotulinumtoxinA selectively. Above all, clinicians must normalize discussions of sexual health and address them proactively as part of routine MS care.
By doing so, healthcare providers move beyond symptom management and help patients reclaim intimacy, dignity, and quality of life.
FAQ
1. Does sildenafil work for erectile dysfunction in men with multiple sclerosis?
Sildenafil has limited effectiveness in MS-related ED, as neurological damage may blunt its vascular benefits. Some men respond, but it is not recommended as a routine therapy.
2. What non-drug therapies help sexual dysfunction in MS?
Evidence supports pelvic floor exercises, aquatic therapy, yoga, and assistive devices such as vacuum suction devices. These approaches improve desire, orgasm, and satisfaction while addressing overall well-being.
3. Are sexual dysfunction treatments safe for MS patients?
Yes. Most interventions, including PDE5 inhibitors, exercise programs, and devices, are safe when supervised. Side effects are usually mild and manageable.
4. Should sexual health be discussed in routine MS care?
Absolutely. Ignoring sexual dysfunction overlooks one of the most important quality-of-life domains for MS patients. Physicians should initiate conversations, normalize the topic, and offer multimodal treatment strategies.